When recovering from soft tissue injuries, the timing of physiotherapy treatment is critical at every stage. Each phase of the healing process—Inflammatory, Proliferative, and Remodelling—requires specific interventions to promote optimal recovery while avoiding setbacks such as stiffness, excessive scar tissue formation, or re-injury. Tightening sensations experienced during recovery serve as signals to guide when and how to intervene, ensuring treatment is effective and aligns with the body’s natural healing cycle.
In a previous post, we looked at the healing process of soft tissue injuries. You can read that here.
Now we’re going to dive into more detail on the timing of treatment, and self-management, during the different phases of recovery that take place during the healing process.
Here’s an integrated look at the importance of timing treatment before, during, and after each phase of the healing process:
1. Inflammatory Phase (0–7 Days): Managing the Acute Stage of Healing
Before the Tightening Begins (Days 0–7)
Why Timing is Important:
– In the initial inflammatory phase, the body is primarily focused on managing the acute injury. Pain, swelling, and inflammation are prevalent, and the area is vulnerable. Overstressing the injured tissue too early could cause further damage, but completely neglecting early treatment can lead to stiffness later on.
It’s important to note though – the body requires inflammation to heal.
Treatment Focus:
– Rest and Protection: The primary focus during this period should be to protect the injured area. Rest and immobilisation, combined with methods such as ice, compression, and elevation, help control inflammation and swelling.
– minimising swelling will in turn minimise the formation of excessive scar tissue.
– Early Pain Management: Pain relief methods are introduced right away, but any movement should be minimised to avoid aggravating the injury.

During the Tightening Phase (Days 7–10)
Why Timing is Important:
– Around day 7–10, as the inflammatory phase subsides and the proliferative phase begins, patients typically experience the first sensation of tightening. This is due to the reduction of swelling, muscle guarding, and early collagen formation. This tightening signals that the tissue is beginning to repair and is ready for careful intervention.
Treatment Focus:
– Gentle Mobilisation: Controlled, pain-free movements should be introduced to prevent stiffness without overstressing the healing tissue.
– Muscle Activation: Light isometric exercises, for example, can be performed to maintain muscle function without stressing the injury.
– Soft Tissue Techniques: Physio and massage therapy can help reduce muscle guarding and improve fluid drainage, aiding early mobility.
After the Tightening Subsides (Days 10–14)
Why Timing is Important:
– Once the initial tightening phase has passed, the injury is in a critical period where stiffness can easily set in if movement isn’t encouraged. However, the tissue is still weak, so exercises should remain gentle and controlled.
Treatment Focus:
– Increase Range of Motion Work: Early flexibility and range of motion exercises help maintain joint movement and prevent adhesions.
– Monitor Tissue Response: Close monitoring ensures that the introduction of mobility doesn’t overstress the tissue, allowing for gradual progression into the next phase.
2. Proliferative Phase (7 Days–6 Weeks): Supporting Tissue Repair and Collagen Formation
Before the Second Tightening (Weeks 1–2)
Why Timing is Important:
– The early proliferative phase (weeks 1–2) is a delicate balance. While early collagen formation is underway, the tissue is still weak and unorganised. This period offers an opportunity to lay the groundwork for flexibility and tissue strength without overstressing the injury.
Treatment Focus:
– Start Flexibility Exercises: Gentle stretching helps guide the proper alignment of new collagen fibres. Timing is crucial here to avoid excessive stiffness while not overstretching the fragile tissue.
– Light Resistance Training: Early strengthening exercises can begin, focusing on low resistance and controlled movements to promote tissue integrity without damaging the new, unorganised tissue.
– Limping on a leg injury, for example, should become much less pronounced by about week 2.

During the Tightening Phase (Weeks 3–4)
Why Timing is Important:
– During weeks 3–4, patients typically experience a second wave of tightening due to collagen maturation. The tissue is becoming stronger, but without timely intervention, the tightening could lead to excessive scar tissue or limited mobility.
– scar tissue shrinks and tightens as it gets older.
Treatment Focus:
– Intensify Flexibility Work: As the collagen matures, flexibility exercises should be intensified to prevent the formation of restrictive scar tissue. Stretching should be progressive but still controlled.
– Introduce More Resistance: Gradually increasing the load through strengthening exercises helps guide proper collagen alignment and tissue function. Resistance exercises should remain controlled to avoid overloading the tissue.
– Manual Therapy for Scar Management: Massage and soft tissue techniques are beneficial for managing any early adhesions and improving tissue elasticity, reducing the feeling of tightness. This encourages more natural movement.
– ideally there is no more limping with a leg injury for example, during this time
After Tightening (Weeks 4–6)
Why Timing is Important:
– Following the tightening sensation of weeks 3–4, the tissue is stronger but still in the process of maturing. This period represents a critical window for solidifying flexibility gains while carefully introducing more loaded, full-range, strength-based interventions.
Treatment Focus:
– Progressive Strengthening: As the tissue continues to strengthen, the intensity of strengthening exercises can increase. Focus on movements that mimic functional activities to prepare the tissue for real-world demands.
– Ongoing Stretching: Stretching and flexibility work should continue, with more dynamic and functional stretching exercises introduced to promote long-term tissue flexibility and alignment.
– Functional Movement Training: Begin incorporating functional exercises to help the patient transition to daily activities and sports-specific movements as the tissue adapts.
– physio and massage can be used to prevent the overtightening of muscles as they begin to strengthen. Muscles tighten as a precursor to strength development.
– Minimising tightness accelerates recovery.
3. Remodelling Phase (6 Weeks–12 Weeks): Restoring Strength and full Function
Before the Final Tightening (Weeks 5–6)
Why Timing is Important:
– As the body approaches the final phase of healing, muscle activation begins in preparation for strength-building. At this stage, patients are on the verge of entering more intensive strengthening exercises, but premature loading could lead to re-injury.
Treatment Focus:
– Prepare for Strengthening: Light functional movements and low-resistance exercises should be continued to prepare the tissue for more intense strengthening work. Timing is key here to prevent muscle imbalances or compensatory movement patterns from developing.
– Maintain Flexibility Work: Regular flexibility and mobility exercises ensure that the tissue remains pliable as the body prepares for strength-building.

During the Final Tightening (Weeks 6–8)
Why Timing is Important:
– During the weeks 6–8 phase, the body’s focus shifts to muscle tightening as a precursor to strength-building. This tightening indicates the muscles are adapting to increased load, signaling that the body is ready for more intensive rehabilitation.
Treatment Focus:
– Strength Training: Strength-building exercises should be introduced carefully, with a focus on progressive resistance. The goal is to build muscle strength without overloading the tissue, which is still remodeling.
– Dynamic and Functional Movements: Incorporate more dynamic exercises that mimic everyday activities or sports-specific movements. This helps the muscles adapt to real-life demands while ensuring that they are properly strengthened.
– Maintain Flexibility: Even as strengthening increases, flexibility exercises should continue to prevent the muscles from becoming overly tight during the strengthening process.
After the Tightening Phase (Weeks 8–12)
Why Timing is Important:
– After the final wave of tightening subsides, the body is focused on long-term tissue remodeling and functional recovery. This phase is crucial for preventing reinjury and restoring full mobility and strength.
Treatment Focus:
– Increase Strength and Endurance Training: As the tissue becomes more resilient, the intensity of strength and endurance exercises can be gradually increased, targeting both the injured area and the surrounding muscles to ensure full recovery.
– Sport-Specific or Functional Training: For athletes or highly active individuals, this is the phase to reintroduce higher-level activities or training that mimics their sport or daily tasks. Timing is essential to prevent reinjury.
– Preventive Maintenance: Regular check-ins with a physiotherapist help ensure that flexibility and strength are maintained, preventing long-term issues or setbacks.
Timing is Key to Successful Recovery
The timing of treatment interventions before, during, and after each tightening phase is critical to ensure that the injured tissue heals effectively while maintaining mobility, flexibility, and strength. By carefully managing each phase of the healing process, physiotherapists, with the help of massage therapy, can guide patients through a smooth recovery, reducing the risk of reinjury, excessive scar tissue, or long-term functional limitations.
Each phase presents a unique opportunity for targeted intervention, and recognising the body’s signals through tightening helps optimise treatment strategies for the best possible outcomes.
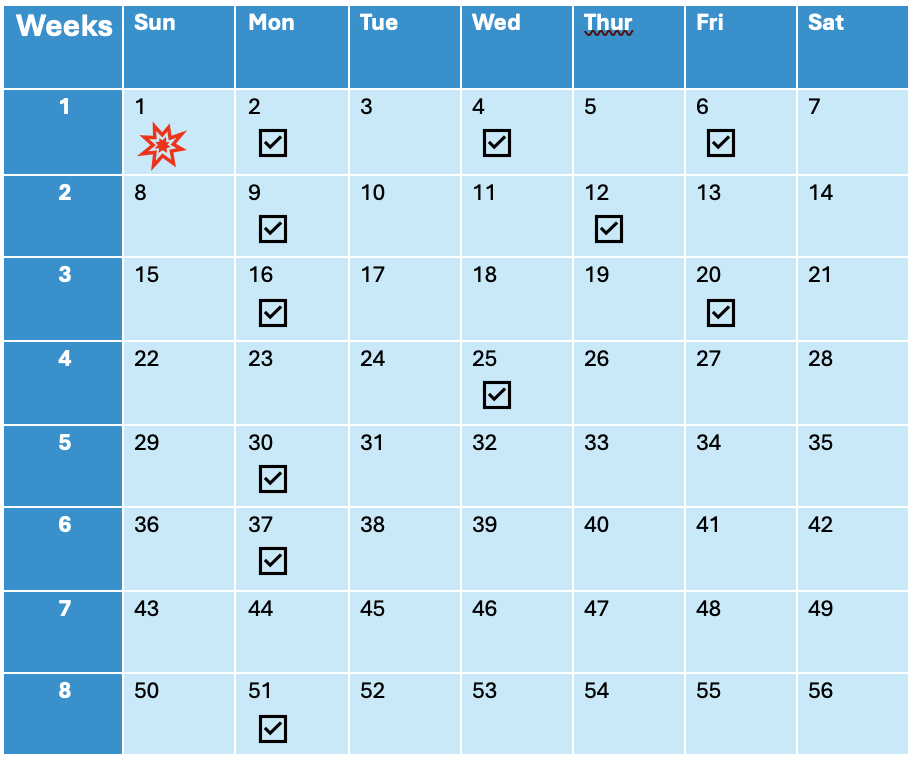
Treatment frequency: Ideal timing to see a therapist.
Calender view. Example: severe calf tear. On crutches until day 10.

Blake Shearsby. Physiotherapist at PhysioCentral. Miranda. The Sutherland Shire.

Graeme Curran. Physiotherapist at PhysioCentral. Miranda.The Sutherland Shire.

Jack Keegan. Physiotherapist at PhysioCentral. Miranda.The Sutherland Shire.