A step-by-step Dietitian’s guide to help you eat safely, prevent nutrient deficiencies, and manage side effects while using Ozempic for Type 2 diabetes.
Why Nutrition Matters on Ozempic
Ozempic (semaglutide) is prescribed to help manage Type 2 diabetes by improving blood sugar control and supporting weight loss.
It works by mimicking a natural gut hormone that helps your pancreas release insulin more effectively, reduces appetite, and slows digestion.
While these changes can improve blood sugar stability and support fat loss, they also make eating feel different.
Some people feel full after just a few bites, forget to eat, or experience nausea, reflux, or constipation.
Over time, this can increase the risk of missing important nutrients and affect your strength, mood, and energy.
Good nutrition on Ozempic isn’t about restriction – it’s about protecting your muscle, gut, and metabolic health while letting the medication do its job.
Common Nutrition Risks on Ozempic
Because Ozempic naturally reduces appetite and slows digestion, you may eat less than your body needs. This can lead to nutrient shortfalls such as:
- Low protein – loss of muscle, fatigue, slower metabolism
- Iron deficiency – tiredness, poor concentration, reduced exercise tolerance
- Calcium & vitamin D gaps – weaker bones, higher fracture risk
- Vitamin B12 deficiency – low energy, mood changes, tingling in hands or feet
- Fibre shortfall – constipation, bloating, gut discomfort
- Electrolyte loss (with nausea or diarrhoea) – cramps, dizziness, dehydration
Recognising these risks early helps prevent complications and ensures Ozempic works safely and effectively.
Practical Steps to Protect Your Nutrition
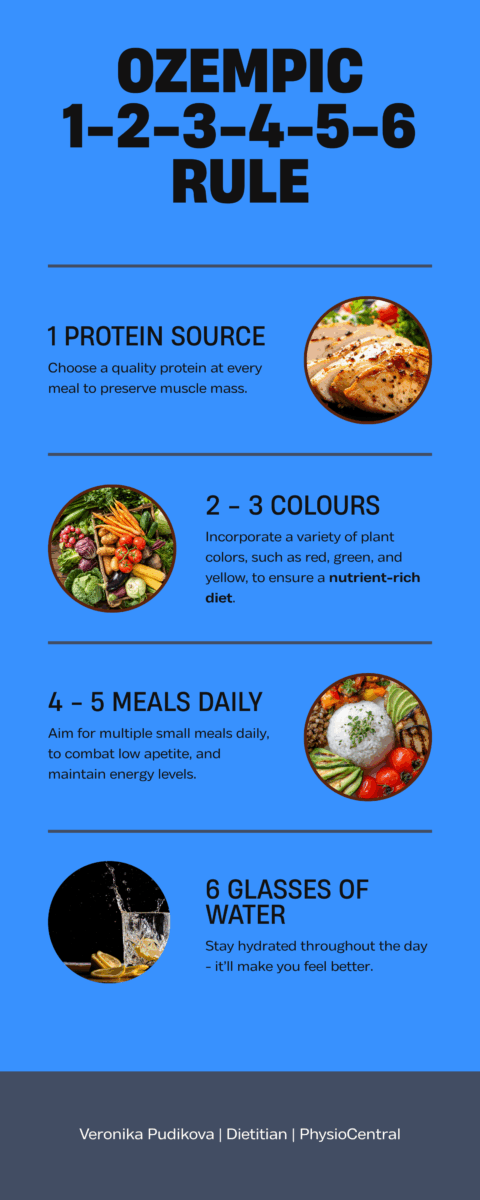
1 Source of Protein at Every Meal
Protein helps preserve muscle, maintain strength, and it is digested slowly, which helps keep blood sugar levels steadier after meals. If your appetite is low, eat protein first.
Daily Example 1:
- Breakfast: 1 egg with wholegrain toast
- Snacks: ½ cup of Greek yoghurt with berries
- Lunch: Palm-sized portion (80 g cooked) of chicken with whole grain salad
- Snacks: Nuts
- Dinner: 65 g lean beef stir-fried with vegetables and brown rice
2–3 Colours of Plants at Every Meal
Colourful vegetables, fruits, nuts, and seeds provide fibre, antioxidants, and key vitamins.
Fibre slows down how quickly food leaves the stomach, meaning glucose enters the blood more steadily.
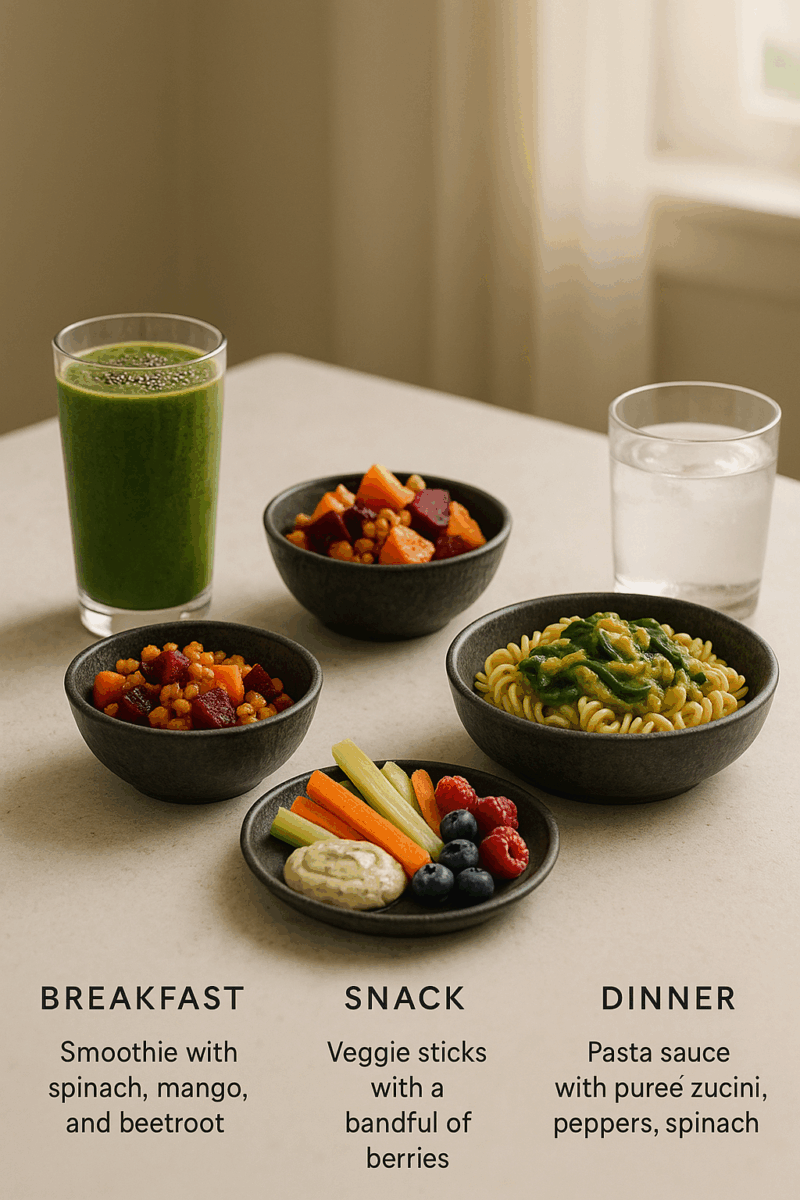
Daily Example 2:
- Breakfast: Smoothie with spinach, mango, and chia seeds
- Snack: Veggie sticks with dip
- Lunch: Roasted pumpkin, sweet potato, and beetroot grain bowl
- Snack: A handful of berries
- Dinner: Pasta sauce with pureed zucchini, peppers, and spinach
4–5 Meals Each Day
Skipping meals raises the risk of fatigue, dizziness, and nutrient gaps. Large meals can cause large blood sugar spikes.
Instead of a large rise and fall after one big meal, smaller portions create gentler changes in blood sugar.
Routine tips:
- Eat breakfast within 2 hours of waking
- Keep to consistent mealtimes
- Set reminders if your appetite is low
6 Glasses of Water Daily
Being well-hydrated supports circulation and helps your body use insulin properly. Drinking enough water also allows your kidneys to flush extra glucose out of the blood through urine.
When you’re dehydrated, constipation is more likely, especially with slower digestion and lower fibre intake. Aim for 2–3 L of fluids each day, consumed steadily rather than all at once.
Fluids that count: herbal teas, tea/coffee in moderation, milk or fortified plant milks, yoghurt drinks, soups, smoothies, and small amounts of fruit juice.
A simple guideline
When to See a Dietitian
See a Dietitian for tailored advice if you notice:
- HbA1c not improving or rising despite medication
- Weight changes that are too fast (>2% loss per week), or stalled after 4 – 6 weeks
- Ongoing nausea, constipation, reflux, or poor appetite
- Unexplained glucose highs or lows despite consistent eating
- You want to build a sustainable long-term food plan for diabetes and weight management
Ozempic is a powerful tool for managing Type 2 diabetes, but it works best alongside good nutrition.
A balanced eating plan helps maintain blood glucose stability, prevent deficiencies, maintain your all important muscle mass, and support long-term energy and wellbeing.
If you’re unsure what to eat – or you feel that food has become confusing or stressful – a Dietitian can help you rebuild a plan that fits your appetite, medication schedule, and lifestyle.
With the right adjustments, you can stay nourished, healthy, and confident while using Ozempic safely.
🧠 Feeling unsure about food, appetite, or nutrition?
👉 Book a session with Veronika for personalised support.
📄 To see her full range of services, visit our Dietetics Clinic in Miranda & the Sutherland Shire services page.

Veronika Pudikova is a Dietitian at PhysioCentral. Miranda. Sutherland Shire