Neck pain and headaches are common ailments that affect millions of people worldwide. They are also the most frequent conditions we treat at PhysioCentral.
Mobility is the first crucial phase in a comprehensive approach to recovery, followed by Flexibility, and finally, Strength.
In this guide, we’ll explore the Mobility Phase and why starting by getting things moving is essential for overcoming neck pain and headaches. While we highly recommend seeking professional treatment, this post will focus on simple, practical movements and exercises during the initial part of the Mobility Phase that you can use to target the critical structures in your neck and spine, setting the platform for a successful recovery.
PhysioCentral’s Three-Phase Treatment Approach
Mobility | Flexibility | Strength
The Three Phases of Recovery
Before we dive into the Mobility Phase, it’s important to understand how it fits into the broader recovery process:
- 1. Mobility Phase: Getting things moving. This phase focuses on restoring movement to stiff joints and soft tissues, reducing pain and spasm, and preparing the body for further rehabilitation.
- 2. Flexibility Phase: Improving range of motion towards normal. The goal is to increase the length and elasticity of muscles and other soft tissues, allowing for more significant movement without discomfort. This phase also prepares the body for the next phase of treatment and rehab.
- 3. Strengthening Phase: Building strength. This final phase reinforces the muscles that support the joints. It’s the weak muscles that often tighten and go into spasm.
For a comprehensive understanding of these phases, refer to our previous post: Understanding Neck Pain and Headaches: A Comprehensive Guide to Lasting Relief
Why Mobility Matters
Understanding Mobility
Mobility refers to the ability of your joints and surrounding tissues to move freely and efficiently with minimal stress and strain.
Mobility vs. Flexibility
Mobility: This phase focuses on joint movement and control within the normal range of motion. Initially, we concentrate on getting the joints moving. As the head and arms move, nerves should slide without restriction or irritation along their pathways. The second part of the Mobility Phase corrects any nerve tension.
Flexibility: Involves the length of muscles and tendons around a joint, allowing all structures to attain a full range of unrestricted motion.
The Importance of Sequence
Attempting to improve flexibility or strength without first addressing mobility can exacerbate existing issues. Tight or immobile joints and tissues are more easily strained, causing an inflammatory response and eliciting the body’s protective muscle spasm.
Muscles go into protective spasm to immobilise the structures of the neck, preventing overstrain and damage. Therefore, restoring mobility is the essential first step in the recovery process.
We need to prepare the area to cope with flexibility work, followed by strengthening, to avoid the setback of triggering overprotective muscle spasm.
Key Structures Involved in Neck Mobility
To appreciate the significance of mobility, it’s essential to understand the structures involved in neck movement:
- Facet Joints
- Intervertebral Discs
- Muscles
- Tendons
- Ligaments
- Nerves
- Blood Vessels
Let’s explore each component, how it contributes to neck function, and how it can lead to neck pain and headaches when mobility is compromised.
Facet Joints: The Hinges of Your Spine
What Are Facet Joints?
Facet joints (also known as zygapophyseal joints) are small joints located between each vertebra on the left and right sides of your spine. They act like hinges, allowing your spine to bend, twist, and move smoothly.
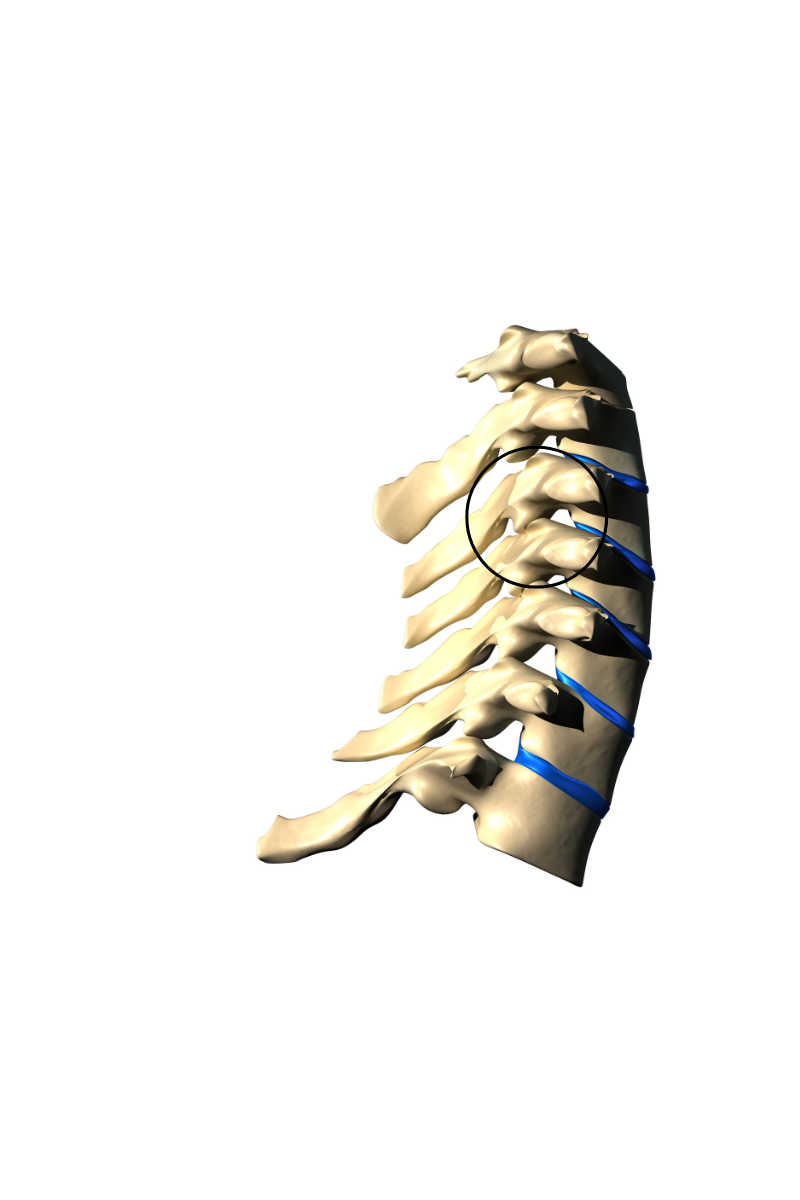
Role in Mobility
Synovial Joints: Facet joints are enclosed in a capsule filled with synovial fluid. This fluid lubricates the joint surfaces, which are covered with cartilage—a smooth, almost ceramic like material that reduces friction. This fluid also contains nutrients to keep the joints healthy.
Movement: Healthy facet joints enable a full range of motion in the neck, including flexion (bending forward), extension (bending backward), rotation, and lateral bending (tilting side to side).
Impact of Immobility
Reduced Synovial Fluid Production: Without movement, synovial fluid production decreases, and the existing fluid becomes more viscous (thicker), reducing lubrication.
Joint Stiffness: Lack of movement leads to stiffness and discomfort. Stiff joints become sensitive and more likely to produce pain.
Formation of Adhesions: Prolonged immobility can lead to the development of adhesions (fibrous bands) within the joint capsule, restricting movement further.
How Facet Joints Contribute to Headaches
Referral of Pain to the Head: Dysfunctional facet joints, particularly in the upper 3 vertebrae of the cervical spine, can refer pain directly to the head, leading to Cervicogenic Headaches – headaches that stem directly from the neck.
Mechanism: The nerves supplying these joints communicate with areas of the brain involved in processing head and facial pain. Irritation of facet joints can cause pain perceived in the back of the head, temples, forehead, or around the eyes. Irritation of these nerves also causes a heightened sensitivity to pain signals, amplifying the feeling of pain. These headaches can become quite severe!
Intervertebral Discs: The Cushions Between Vertebrae
What Are Intervertebral Discs?
Discs are soft cushions with a gel like inner core located between the vertebrae. They act as shock absorbers and also allow the spine to be flexible.
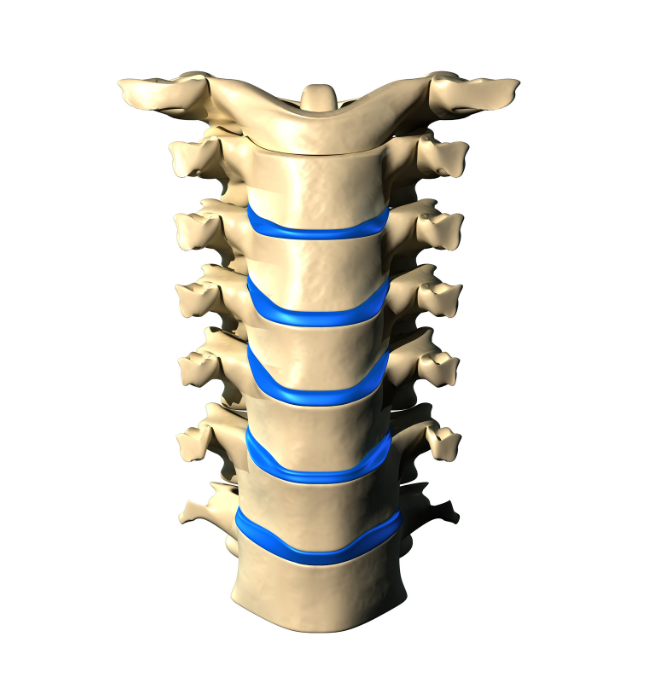
Role in Mobility
Shock Absorption: Discs absorb impact during movement.
Facilitating Movement: The bony vertebrae sit on a cushion that allows the spine to bend and twist smoothly.
Impact of Immobility
Reduced Nutrition: Discs rely on movement rather than circulation to receive nutrients.
Degeneration: Lack of movement can contribute to disc degeneration, which leads to decreased flexibility and potential pain. Degeneration is really just a decrease in the disc’s suppleness or plumpness—a bit like the internal version of wrinkles on the skin.
How Discs Contribute to Headaches
Disc Degeneration and Nerve Irritation: Degenerated or herniated discs can irritate and compress nearby nerves, leading to pain that radiates to the head.
Pressure on Nerves: This compression can cause headaches by irritating nerves that have a direct pathway to the head.
Muscles, Tendons, and Ligaments: The Support System

Muscles
Muscles generate force to move and stabilise the neck. Some key neck muscles include the sternocleidomastoid, trapezius, levator scapulae, and scalenes.
Tendons
Tendons attach muscles to bones, transmitting the force necessary for movement, and postural stability.
Ligaments
Ligaments connect bones to other bones, providing stability to the joints.
Role in Mobility
Muscles and Tendons: Facilitate movement by contracting and relaxing.
Ligaments: Stabilise joints during movement.
Impact of Immobility
Muscle Tightness: Inactivity can lead to shortened, tight muscles.
Reduced Elasticity: Tendons and ligaments can lose elasticity, making movements stiff and uncomfortable.
Sensitivity: Stiff, tight soft tissue becomes sensitive, and pain producing.
How Muscles, Tendons, and Ligaments Contribute to Headaches
Muscle Tension and Trigger Points: Muscle tightness or spasm can lead to Tension Headaches, typically felt as a dull ache or pressure band around the head.
Attachment Points: Tight muscles, especially those attaching at the base of the skull (like the suboccipital muscles), can cause pain in the back of the head.
Inflammation at Tendon Attachments: Overuse or strain can inflame tendons where they attach to the skull, contributing to headaches. They can become so inflamed, swollen, and sensitive, that even resting your head on a pillow generates a headache.
Ligament Strain: Injured or overstretched ligaments can trigger pain receptors, leading to neck pain and headaches.
Nerves: The Communication Pathways
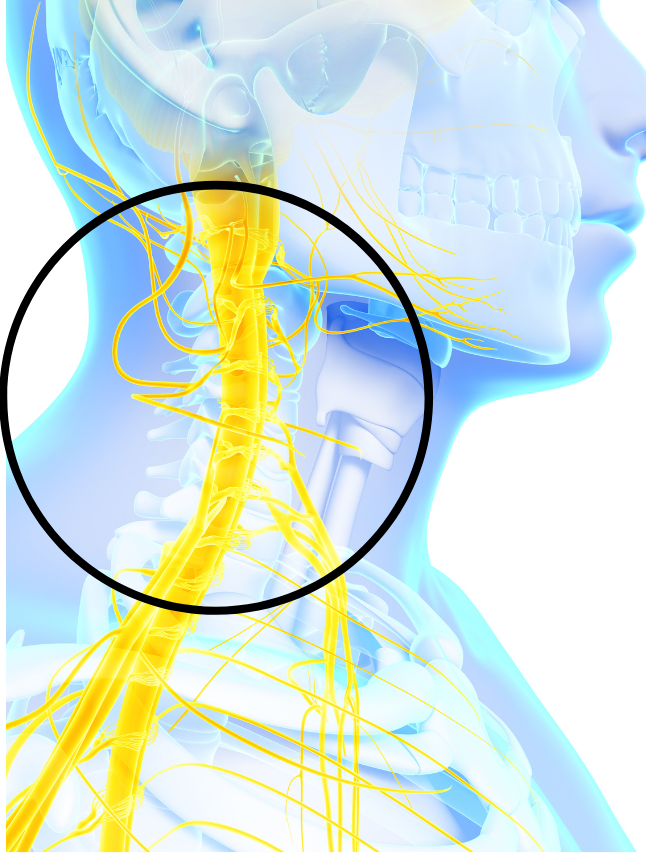
Role in Mobility
Signal Transmission: Nerves carry signals between the brain and muscles, coordinating movement, and activating postural muscle tension to support the shape of the spine.
Nerve Gliding: Nerves need to move or glide slightly within surrounding tissues during joint movement of the neck, shoulders, and arms.
Impact of Immobility
Restricted Nerve Movement: Lack of mobility can lead to adhesions around nerves, limiting their ability to slide.
Nerve Irritation: This can cause pain, tingling, or numbness and may trigger protective muscle guarding, further restricting movement.
How Nerves Contribute to Headaches
Nerve Compression and Irritation: Compressed or irritated nerves in the neck can cause pain that radiates to the head.
Occipital Neuralgia: Irritation of the occipital nerves (base of the head) can lead to sharp, shooting pains in the back of the head and behind the eyes.
Protective Spasm: Lack of nerve mobility leads to protective spasm of muscles in the neck and upper shoulders, further exacerbating symptoms.
Blood Vessels: Nourishing the Tissues

Role in Mobility
Supply of Nutrients and Oxygen: Blood vessels deliver essential nutrients and oxygen to muscles, discs, nerves, and other tissues.
Removal of Waste Products: They help eliminate metabolic waste, including inflammatory substances, from these tissues.
Impact of Immobility
Reduced Circulation: Inactivity can decrease blood flow, slowing down healing processes and contributing to muscle spasm and feelings of stiffness. It can also lead to a buildup of inflammation as the circulation has difficulty clearing it out.
How Blood Vessels Contribute to Headaches
Vascular Changes: Tight neck muscles can compress blood vessels, reducing blood flow to the head and potentially triggering headaches.
Vascular Headaches: Improved mobility can enhance circulation, reducing the likelihood of vascular headaches.
Consequences of Reduced Mobility
When mobility is compromised, it sets off a chain reaction:
- Joint Stiffness: Leads to reduced movement and pain.
- Muscle Tightness: Muscles shorten and become tight, further limiting mobility. The tighter muscles get – the more pain they produce.
- Nerve Irritation: Restricted movement can irritate nerves, causing pain and discomfort.
- Protective Muscle Guarding via Spasm: The body responds by tightening muscles to protect the area, perpetuating the cycle of pain and immobility.
- Headaches: Dysfunction in any of these neck structures can lead to headaches, amplifying pain and triggering off an even stronger protective muscle spasm, which in turn enhances all of the above processes, and the cycle repeats.
The Mobility Phase: Getting Things Moving
Goals of the Mobility Phase
Restore Joint Movement: Enhance the movement of facet joints and other joint structures. Just getting the joints moving again stimulates the joint membrane to produce more synovial fluid, lubricating the joint surfaces and allowing frictionless movement to return.
Reduce Muscle Tightness: Gently ease muscles out of a tight, protective state, reducing pain and compression.
Promote Nerve Gliding: Encourage smooth movement of nerves within and along their pathways.
Increase Circulation: Boost blood flow to affected areas to clear out inflammation, which helps ease spasm and promote healing.
Strategies for Improving Mobility
Restoring mobility often requires a combination of professional treatment and self-directed exercises. Here’s how a physiotherapist might approach the Mobility Phase:
Physio Treatment
Neck and Upper Shoulder Massage: The first step is to address the tight, sore muscles that are typically in a state of protective spasm. A physio will use massage techniques to relax these muscles, reducing pain and allowing for better movement. A tight muscle can act like a tourniquet on itself, restricting blood flow and trapping inflammation within the muscle—leading to those tight, sore muscles you feel in your upper shoulders and neck.
It’s important to note, however, that treatment must initially avoid loosening up the Trapezius muscle (the muscle of the upper shoulders). Even though this muscle can feel like it’s the source of a lot of pain and ‘needs a massage’, doing so prematurely will exacerbate your symptoms. We must loosen up the other structures first somewhat, before we attack the upper traps. Funnily enough though, once the other structures are freed up, trap spasm usually settles quickly of it’s own accord. Trap spasm is a symptom, not the root cause of your pain.
Joint Mobilisation: Next, attention is drawn to the joints themselves. Physios use gentle and accurately directed bouncing, like repetitive pressure, to get the rigid facet joints moving again. This technique helps restore normal joint function, stimulates synovial fluid production, and alleviates stiffness. Stiff joints cause pain – so this is very important.
Nerve Mobility: After working on the muscles and joints, the physiotherapist will check the sensitivity and tightness of the nerves that exit the spine. These nerves pass through several muscles, travel under the collarbone, navigate through shoulder structures, and extend down the arm to the wrist and hand. Assessing and addressing nerve tightness is crucial for reducing pain and improving overall mobility. If the nerves are compromised in any way, protective muscle spasm will be triggered to lock everything down and prevent the nerves from being overstretched – once again leading to those tight, sore neck and upper shoulder muscles.
With the right kind of treatment, most of our patients notice a significant improvement in symptoms in as little as 1–3 sessions, carried out over a 10 – 14 day period. Headaches become less intense, don’t last as long, and become far less frequent.
The Exercise Program
Part 1: Neck Mobility
In addition to professional treatment, incorporating simple exercises into your daily routine can significantly enhance mobility. Treatment is just a push in the right direction. Mobility will only really improve with high volume repetitive movements of the neck. Here are some exercises we recommend:
Video below
1. Chin Tucks
How to Do It:
While keeping your eyes forward, pull your chin straight back, creating a “double chin.”
Hold for a moment and release.
Repetitions: Repeat 3 times.
Benefits: Mobilises and relaxes the deep neck muscles, promotes improved alignment, and can reduce headaches stemming from nerve and muscle strain.
2. Neck Flexion
How to Do It:
Slowly lower your chin toward your chest, allowing the weight of your head to create a gentle movement.
Repetitions: Repeat 3 times.
Benefits: Mobilises facet joints, encourages synovial fluid production, reduces stiffness, and can alleviate headaches caused by joint stiffness.
3. Lateral Neck Tilts
How to Do It:
Tilt your head toward your right shoulder, keeping your shoulders relaxed.
Return to the centre and repeat on the left side.
Repetitions: Repeat 3 times on each side.
Benefits: Improves side-to-side movement, reduces muscle tightness, and can relieve tension-type headaches stemming from muscle strain.
4. Neck Rotation
How to Do It:
Gently turn your head to look over your right shoulder.
Return to the centre and turn to look over your left shoulder.
Repetitions: Repeat 3 times on each side.
Benefits: Enhances rotational mobility, promotes nerve gliding, and reduces nerve irritation that can lead to headaches.
5. Shoulder Rolls
How to Do It:
Roll your shoulders upward, backward, downward, and forward in a smooth, circular motion.
Repeat 3 times.
Then, do it in the opposite direction.
Benefits: Relieves tension in the neck and shoulders, improves circulation, and can alleviate headaches associated with muscle tension and vascular constriction.
Repeat these exercises, one after the other, 3–5 times for best results.
Perform several times per day.
Tips for Effective Mobility Practice
Gentle Movements: Avoid pushing into pain. Movements should be comfortable and controlled.
Frequent Repetition: Aim to perform these exercises multiple times throughout the day.
Incorporate them into your routine: Do them during ad breaks while watching TV, for example.
Stay Relaxed: Keep your shoulders down and muscles relaxed to prevent unnecessary tension.
Consistency is Key: Regular practice leads to gradual improvement.
We recommend performing these exercises multiple times daily. For example, gently perform them at every set of red traffic lights or when stuck in traffic. In some cases, people end up doing these exercises 20, 30, or even 40 times a day. If you keep the neck moving, you can imagine how difficult it would be for it to tighten and compress. As your neck pain and headaches resolve, stick to this habitual movement pattern—it works even better as a preventative.
It’s essential to build up to this amount gradually. Most people start at just 5 or 6 times per day and take weeks to increase to a higher volume. We need to give the newly mobilising joints time to produce enough fluid to cope and for the muscles to get used to contracting and relaxing rather than just holding in a contracted state 24/7—which is what muscle spasm tends to do.
The body is an adaptive machine if we give it time to adapt.
It adapts to inactivity by tightening up. Now, it needs time to adapt to an increase in mobility exercises.
The trick is to perform all exercises gently and, eventually, repetitively, to calm everything down.
Avoiding Common Mistakes
Forcing Movements: Don’t push your neck beyond its comfortable range. Doing so can cause overstrain and trigger muscle spasm.
Holding Positions: Remember, this phase is about movement, not sustained stretches. Muscles like sustained stretch, but joints and nerves don’t. They need repetitive movement. Once mobile, it’ll be safe to stretch during the Flexibility Phase.
Irregular Practice: Sporadic efforts won’t yield significant results. Consistency matters.
Ignoring Pain Signals: If a movement causes sharp pain, you’re overdoing it. You may feel a gentle strain or stretch sensation—even a dull ache is permitted—but never sharp pain.
Next Step: Nerve Mobility Exercises (Neurodynamics or Nerve Flossing)
Part 2: Nerve Mobility
Part 2 of the Mobility Phase addresses any nerve tightness or decreased nerve mobility via a series of exercises known as nerve glides or nerve flossing. These exercises help improve the mobility of your nerves, reducing irritation and enhancing their ability to glide smoothly through surrounding tissues.
Why Nerve Mobility Matters
Reduces Nerve Irritation: Alleviates pain, tingling, or numbness.
Enhances Nerve Function: Promotes healing.
Decreases Protective Muscle Guarding: Reduces the likelihood of muscles tightening around irritated nerves.
Video below
Nerve Mobility Exercises
1. Nerve Slider
How to Do It:
Stand with your right hand up at shoulder level, palm facing up as if holding a tray.
Turn your head to the left (away from your hand).
Straighten your right arm out to the side while rotating your head to the right to look at your hand.
Repetitions: Repeat 3 times.
Benefits: Mobilises the nerves of the brachial plexus, reducing tension and improving nerve glide.
2. Nerve Tensioner
How to Do It:
Start with your right hand in the same position, palm up, looking at your hand.
Straighten your arm out to the side as before, but this time turn your head to the left (away from your hand).
Repetitions: Repeat 3 times.
Benefits: Gently tensions the nerves to improve mobility and reduce irritation.
3. Wall Stretch with Head Turn
How to Do It:
Place your right hand against a wall at shoulder height, palm flat, fingers pointing backward.
Turn your head away from your right arm.
Repetitions: Repeat 3 times.
Benefits: Stretches and mobilises the brachial plexus nerves.
4. Wall Stretch with Head Tilt
How to Do It:
Keep your right hand against the wall.
Tilt your head to the left (away from your right arm).
Repetitions: Repeat 3 times.
Benefits: Enhances nerve gliding by combining arm and neck movements.
Repeat the entire sequence 3–5 times per day.
Tips for Performing Nerve Mobility Exercises
Gentle Movements: Perform the exercises slowly and gently. Avoid any rapid or jerky movements.
No Overstretching: You should feel a mild stretch or tension, not pain. Stop the exercise if you experience sharp pain, numbness, or increased tingling.
Breathing: Maintain steady breathing throughout the exercises to promote relaxation.
Consistency: Incorporate these exercises into your daily routine for optimal benefits.
Progressing to the Flexibility Phase
The Mobility Phase (joints and nerves) takes up to two weeks – in severe cases – before our patients can advance to the Flexibility Phase. The speed of recovery depends on many factors, such as posture, daily sitting time, exercise routine, age, and the length of time you’ve spent putting up with symptoms.
The Flexibility phase takes 1 – 2 weeks.
Prepare for the final phase of recovery – Strengthening: Improved flexibility sets the stage for effective strength training.
Understanding the Sequence: Mobility → Flexibility → Strength
Mobility First: Ensures joints and tissues can move freely.
Flexibility Second: Increases the range of motion by lengthening muscles and tendons.
Strength Last: Builds postural muscle strength and endurance to support the spine and weight of the head.
Skipping steps or altering this sequence can lead to setbacks, as the body may not be ready for the demands of flexibility or strength training without first ensuring adequate mobility.
Joints and Nerves Require Mobility First: They dislike being stretched in a sustained fashion or too aggressively. They need gentle, repetitive movement to function properly and calm them down and avoid triggering protective spasm again.
Muscles Love Gentle Stretching: It relaxes them, but we must first loosen up the tight joints and nerves so they can cope with the stretching introduced in the Flexibility Phase.
Weak Muscles Tighten with Premature Strengthening: Introducing strength work too early just causes the tight bits to get tighter, worsening your symptoms. We need to work through the previous steps so the body can handle the strengthening phase.
Remember this rule:
“We need to loosen up the tight bits before we can strengthen the weak bits.”
This applies to any injury, ache, or pain—not just the neck.
When to Seek Professional Help
Persistent Pain: If pain doesn’t improve with mobility exercises.
Severe Pain: There’s no need to put up with it. Get it sorted!
Unusual Symptoms: Such as worsening headache, numbness, tingling, or weakness in the arms.
Uncertainty: If you’re unsure about how to perform exercises correctly.
To Accelerate Recovery: Professional help can dramatically speed up recovery.
We recommend everyone seek attention for neck pain, especially when headaches are involved. However, we also realise not everyone wants to follow this path. Please take heed of the above advice and consult a professional if needed.
To sum it all up
The journey to overcoming neck pain and headaches begins with getting things moving. The Mobility Phase is all about restoring natural movement to your neck and spine, which is essential before advancing to flexibility and strength training. With a bit of knowledge, focusing on the practical movements introduced in this guide, and understanding how each structure contributes to headaches, you’ll be much better placed to address the root cause of your problem, not just temporary symptomatic relief.
Remember, consistency and patience are key. We’re talking about a permanent cure. You’re the Tortoise, not the Hare.
Gentle, regular movements performed throughout the day can lead to significant improvements over time. By respecting the sequence of recovery – mobility first, then flexibility, and finally strength – you set yourself up for lasting success and a complete loss of symptoms.

Blake Shearsby. Physiotherapist at PhysioCentral. Miranda. The Sutherland Shire.

Graeme Curran. Physiotherapist at PhysioCentral. Miranda.The Sutherland Shire.

Jack Keegan. Physiotherapist at PhysioCentral. Miranda.The Sutherland Shire.

Jasmine Watson. Physiotherapist at PhysioCentral. Miranda.The Sutherland Shire.
Disclaimer: This guide is only informational and does not substitute professional medical advice. Always consult a qualified healthcare provider before starting any new exercise regimen, especially if you have existing health conditions or concerns.