Why eating “smarter” matters on Ozempic
Ozempic doesn’t just curb appetite – it changes how your body processes food.
It slows digestion, steadies blood sugar, and reduces hunger signals.
That means what and how you eat becomes just as important as how much you eat. Meals that once felt fine might now trigger nausea, reflux, or fatigue. Skipping meals can also backfire, leading to sugar dips, dizziness, or muscle loss over time.
For people with type 2 diabetes, nutrition balance is even more critical.
Ozempic improves insulin sensitivity and helps stabilise glucose levels, but inconsistent eating can still cause highs, lows, or nutrient gaps. Matching food timing, carb quality, and protein intake with your medication helps protect your energy, muscle mass, and long-term metabolic health.
That’s why eating on Ozempic isn’t just about eating less – it’s about eating smarter. Smaller portions, balanced carbs, and fibre-rich meals work with the medication to keep your blood sugar, digestion, and energy steady.
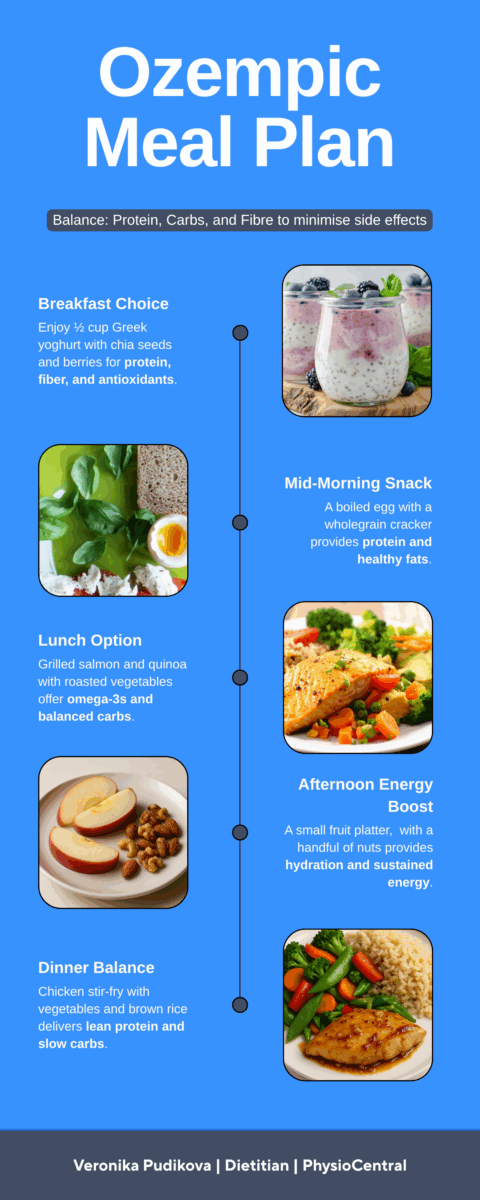
An example day of eating on Ozempic
Breakfast
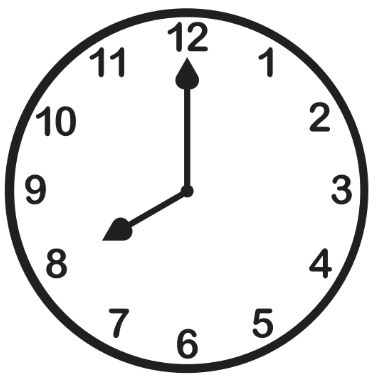
½ cup Greek yoghurt + 2 Tbsp chia seeds + berries • Protein supports muscle mass & slows sugar absorption • Chia adds fibre for smoother blood sugar response • Berries are lower-GI fruits with antioxidants, vitamins and fibre
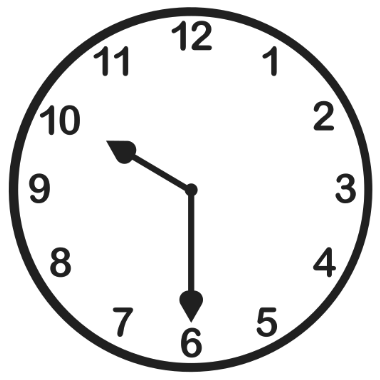
Mid-morning snack
1 boiled egg + wholegrain cracker + 1 Tbsp hummus • Protein and fat in egg and hummus stabilise sugar spikes • Wholegrain carb for slow sugar breakdown
Lunch
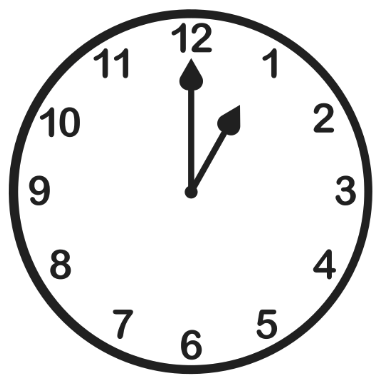
Grilled salmon (80 g) + ½ cup quinoa + roasted veg • Salmon provides protein + omega-3s for insulin sensitivity • Quinoa offers balanced carb + protein with a low-GI profile • Non-starchy veg add fibre and help regulate post-meal glucose
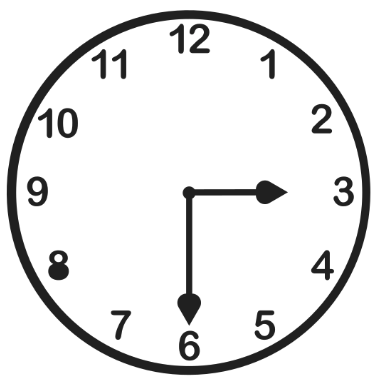
Afternoon snack
1 small fruit + handful of nuts • Fruit for fibre-packed carbs + hydration (low-GI like apple or pear) • Nuts provide protein, healthy fat, and minerals (e.g., magnesium)
Dinner
Chicken breast (65 g) soy–ginger–garlic stir-fry + veg + ½ cup brown rice • Lean protein helps stabilise evening glucose • Brown rice + fibre-rich vegetables provide slow-release carbs
Daily ballpark (example only)
≈ 1,250 kcal, 76 g protein • Prioritises protein and fibre to manage glucose uptake • Smaller portions respect slowed digestion from GLP-1 RAs • Balanced carb distribution reduces highs/lows across the day
Essential adjustments to eat well on Ozempic
- Carb timing & distribution: Review intake and glucose logs → spread carb servings evenly across the day (2–4 per meal).
- Food choices: Prioritise intact whole grains, legumes, low-GI fruits → offer swaps aligned with culture and preferences.
- Carb portioning: Use the carb spoon/exchange method (~15 g carbohydrate) → set an individual allowance.
- Pairing: Combine carbs with lean protein or healthy fats → use meal/snack templates for steady glucose.
- Symptoms & tolerance: Screen nausea, reflux, constipation, fatigue → adjust meal size/texture, fibre type, hydration, and fat.
- Hydration: Estimate daily fluid needs → steady sipping; avoid hidden carbs in drinks.
- Labs & monitoring (with GP): Track HbA1c, iron, B12, vitamin D, renal function → guide food sources and consider Diabetes-Specific Nutritional Formula if needed.
- Medication context: Consider Ozempic dose timing and other meds → prevent hypo risk; adapt meals on injection days.
- Lifestyle fit: Factor activity, cooking skills, budget, schedule → redistribute carbs on training days; suggest portable snacks.
- Sustainability & enjoyment: Keep favourite foods in controlled amounts → adapt for long-term adherence and quality of life.
When to see a dietitian
- No energy to live your life – dragging through the day; workouts feel impossible.
- Food feels confusing or exhausting – skipping meals, then crashing later.
- Your stomach is running the show – nausea, reflux, constipation, bloating.
- Your sleep is broken – waking at 3 am wired or hungry.
- Blood sugars are all over the place – big spikes, sudden dips, fear of eating.
- You’re losing weight too fast – along with grip strength, mood, or hair quality.
- You keep cancelling on life – avoiding coffee with friends, exercise, family dinners.
- You’re doing this alone (you don’t have to!) – blogs and apps haven’t solved it.
What Veronika does (and why people feel better)
- She listens first. Your symptoms, appetite window, routine, culture, budget—what real life looks like.
- She personalises the “tiny-serve” plan. Small portions at the right times so you feel steady – without bigger plates.
- She uses your data. Meter/CGM screenshots, weight trend, and key labs to dial in carb “spoon” sizes and protein pairings.
- She troubleshoots gently. Nausea, constipation, sleep, energy – small tweaks that make eating easy again.
- She keeps you safe. If something looks off, she quickly liaises with your GP.
If you’re losing weight but losing yourself, that’s the moment to get help.
🧠 Feeling unsure about food, appetite, or nutrition?
👉 Book a session with Veronika for personalised support, and a mini meal map you can start the same day.
📄 To see her full range of services, visit our Dietetics Clinic in Miranda & the Sutherland Shire services page.

Veronika Pudikova is a Dietitian at PhysioCentral. Miranda. Sutherland Shire
Further reading
• How Ozempic, Wegovy and Mounjaro Change Your Appetite, Digestion and Weight
• The Ozempic Nutrition Toolkit: What to Eat (and Why)
Dietitian and nutrition support for Ozempic users in Miranda and the Sutherland Shire.